Introduction
Ovarian Hyperstimulation Syndrome (OHSS) is a potentially serious and sometimes life-threatening complication associated with assisted reproductive technologies, particularly in vitro fertilization (IVF). This articles focuses on the identification of OHSS risk factors and current predictive models to guide individualized ovarian stimulation to enhance both safety and efficacy in fertility care. It is without doubt that OHSS remains the most serious complications of controlled ovarian stimulation, underscoring the great relevance of preventive strategies in clinical practice.
Pathophysiology
OHSS is characterized by exaggerated ovarian response to exogenous gonadotropins, leading to increased vascular permeability, fluid shifts, and a range of systemic symptoms. The primary cause of this is attributable to increased VEGF production occasioned by the high number of luteinized granulosa cells triggered by endogenous human chorionic gonadotropin. The clinical presentation can vary widely, from mild abdominal discomfort to severe ascites, thromboembolism, and even multi-organ dysfunction.
Primary intervention
Primary intervention is the avoidance of the challenge in the first place. The identification of potential moderate-high risk cases is central to any OHSS prevention programme, especially as we promote OHSS free clinic in Ghana. Early identification of individuals at risk is therefore crucial to improving patient outcomes, minimizing complications, and optimizing treatment protocols.
Primary risks factors
These are pre-existing factors which should be identified and stratified in all patients prior to ovarian stimulation. The most objective predictive markers are the baseline Antral Follicle Count (AFC) of more than 24 and/or Anti-Mullerian Hormone (AMH): of greater than 3.4ng/ml.
1. High baseline AFC more than 24
2. High AMH greater than 3.4ng/ml
3. The presence of PCOS and other causes of anovulation (besides follicular depletion)
4. Previous history of OHSS
5. Young age, typically < 30 years due to higher ovarian reserve and increased sensitivity to gonadotropins
6. Low body weight – more sensitive to gonadotropins
7. Black race - at increased risk than Caucasians
8. High risk genetic predictors include N680S variant and FLT4 gene variants
Secondary factors
These are the cycle related factors identified during the ART process, especially during ovarian stimulation and the processes thereafter. These factors include:
1. Rapidly rising estradiol (E2) levels. Whenever E2 levels are greater than 5000ng/l there is a high likelihood of moderate-severe OHSS.
2. A large number of developing follicles on the day of hCG administration (>19 follicles with a diameter of 11 mm (Griesinger, 2016)
3. Large number of oocytes retrieved- retrieval of more than 15 oocytes significantly elevates this risk, with the likelihood increasing markedly beyond 20 oocytes (ESHRE, 2020; Griesinger et al., 2016)
4. Use of agonist protocol (antagonist protocol has been found to be protective)
5. Use of HCG for ovulation trigger or luteal support
6. Pregnancy following ovarian stimulation
7. High cumulative gonadotropin dose
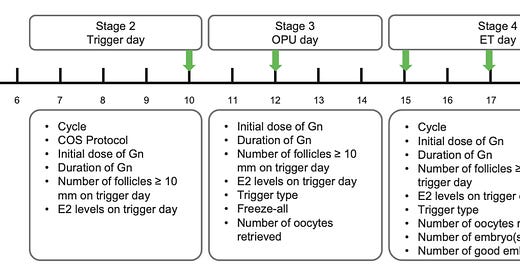
A recent publication by Cao et al., summarizes these risks in a single diagram reproduced below:
Cao et al., 2024 OHSS Risk Assessment Index
Conclusion
OHSS prevention in ART practice begins with the identification of both primary and secondary risk factors and integration of this knowledge into routine clinical assessment to advance safer and more individualized ovarian stimulation protocols. In line with the global movement toward OHSS-free clinics, especially within the context of fertility care in Ghana, a proactive and structured approach to risk identification must become standard practice to protect patient health while maintaining high treatment success rates.




Thanks Dr Amoateng for such an insightful write up, it's really an eye opener for us in the area of fertility.
Thank you so much