Quiz Master: Dr. Bernard Brewu, REI Senior Resident, KATH
1. Is routine hysteroscopy required prior to IVF-ET?
Answer:
Routine hysteroscopy is not mandatory before IVF-ET. However, some form of endometrial cavity assessment is necessary during the patient work-up. This can be achieved through:
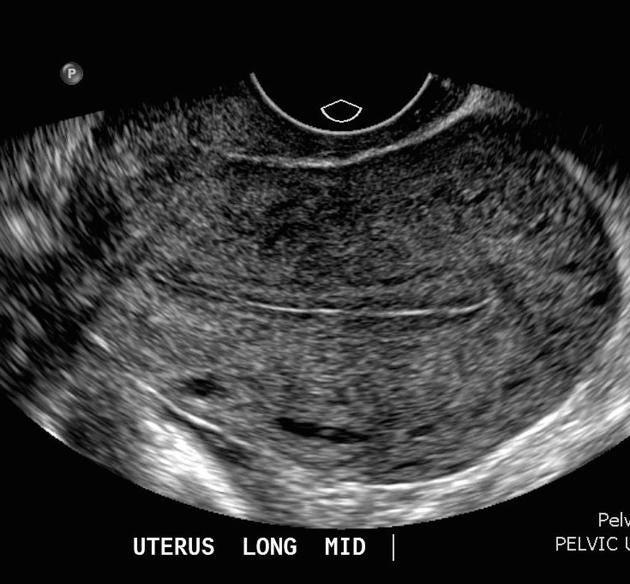
Transvaginal Sonography (TVS): Adequate for most patients.
Saline Infusion Sonography (SIS): May be indicated for further evaluation.
Hysteroscopy: Reserved for cases with specific indications based on the patient’s history and examination findings.
2. What are the options available if the catheter doesn’t pass during a mock transfer?
Answer:
In cases where catheter passage is challenging, consider the following:
a. Adjust or change the speculum size for better visualization of the cervical lips.
b. Ensure the bladder is adequately full if the uterus is anteverted.
c. Reposition the patient (e.g., McRoberts position for anteverted uterus).
d. Use a stylet with the ET catheter for guidance.
e. Perform gentle cervical dilation with an os-finder or a small dilator.
f. For further dilation, perform the procedure in a theater setting with adequate analgesia or anesthesia.
g. If the uterus is retroverted, empty the bladder to improve access.
h. Avoid holding the cervix with a tenaculum or vulsellum, as it can trigger contractions.
i. For recurrent issues, place a silk 0 or 1 stitch on the cervical lip during the mock transfer to assist with traction during the actual transfer
3. What should you do if a myoma is detected at the internal os during a mock or actual transfer?
Answer:
a. Use a stylet with the ET catheter.
b. Employ an os-finder to navigate around the obstruction.
c. Consider freezing the embryos and deferring the transfer to manage the fibroid before proceeding.
4. What if the tip of the catheter isn’t visible on ultrasound during mock or actual transfer?
Answer:
a. Call for assistance.
b. Adjust ultrasound scan settings for better visualization.
c. Verify the catheter's placement; it may be bent backward towards the vagina

5. What do you do if the bladder is too full or underfilled during the procedure?
Answer:
a. If the bladder is overfilled, catheterize and drain excess urine.
b. If the bladder is underfilled, consider filling it manually.
6. How do you handle a patient with anxiety or vaginismus?
Answer:
a. Consider anxiolytics or light sedation.
b. Routine sedation is not recommended but may be considered for selected patients.
7. What if the cervical os isn’t found during a mock transfer?
Answer:
If the os is not identifiable and patient is not yet menopausal:
a. Defer the mock transfer until the next menstrual cycle.
b. During menstruation, locate the os by observing the point of discharge.
c. Mark the location in the patient’s folder or place a silk suture near the os for guidance during the actual transfer.
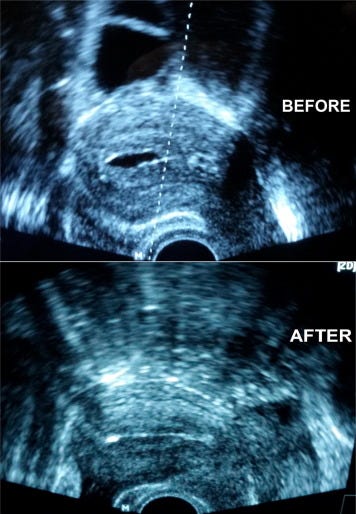
8. What should you do when fluid is observed in the endometrial cavity during the actual transfer?
Answer:
a. If the fluid collection is less than 2 mm, proceed with the ET.
b. Rule out hydrosalpinx as a possible cause.
c. Adjust hormonal therapy: Increase progesterone and reduce estrogen levels.
d. For persistent or significant fluid collection, freeze the embryos, consider drainage, and conduct an endometrial biopsy.
e. Use a natural cycle to avoid hormone-induced fluid accumulation
Fluid in the cavity at ET: Practical Problems in Assisted Conception , pp. 79 - 85 DOI: https://doi.org/10.1017/9781108149891.018 Publisher: Cambridge University Press, 2018
Fluid in the cavity at OPU: aspiration. https://doi.org/10.1016/j.mefs.2018.04.012
Reading for practitioners [ESSENTIAL]
The ASRM standard embryo transfer protocol template: A committee opinion is a good paper to review. The ASRM Standard Embryo Transfer Protocol Template provides associated evidence for all practices to use to model their own standard protocol
.








I believe McRoberts was recommended for retroverted uterus when other easer options have failed.